Ovarian Cancer Screening: A Comprehensive Guide
Ovarian Cancer Screening
Ovarian cancer is a disease that has the potential to be life-threatening and impacts numerous women around the globe. Early detection and timely intervention play a crucial role in improving the prognosis and survival rates of ovarian cancer patients. In this article, we will delve into the topic of ovarian cancer screening, exploring its importance, methods, and considerations. By understanding the available screening options, women can make informed decisions about their health and take proactive steps toward early detection.
Understanding Ovarian Cancer Screening
What is Ovarian Cancer?
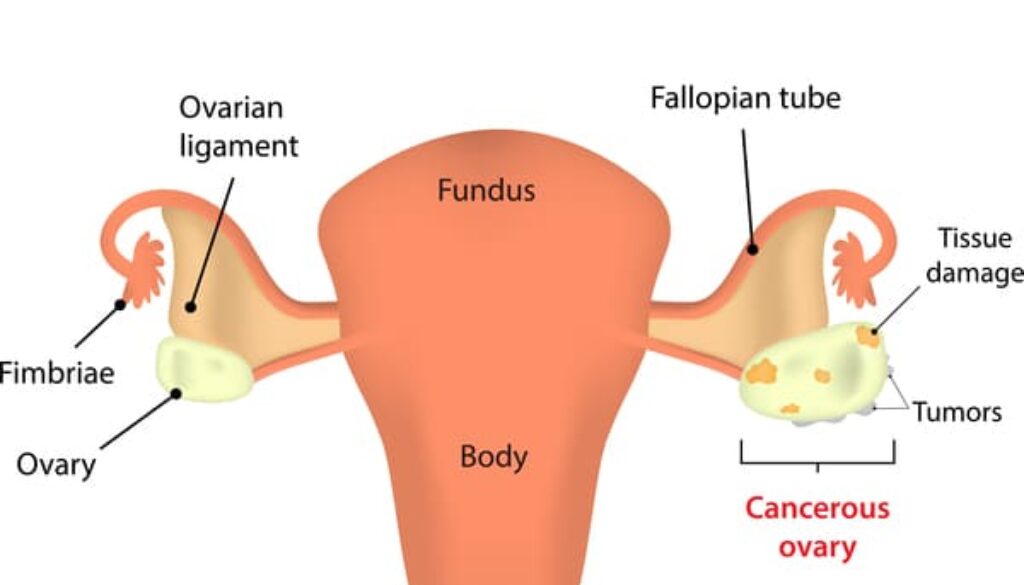
Ovarian cancer is a type of cancer that originates in the ovaries, the reproductive organs responsible for producing eggs. It occurs when abnormal cells in the ovaries grow and divide uncontrollably, forming tumors. Ovarian cancer can spread to nearby organs and, if left untreated, metastasize to distant sites in the body.
Causes and Risk Factors
The exact cause of ovarian cancer remains unknown, but certain risk factors have been identified. These include a family history of ovarian or breast cancer, inherited gene mutations (such as BRCA1 and BRCA2), increasing age, hormone replacement therapy, and obesity. However, it’s important to note that having one or more risk factors doesn’t guarantee the development of ovarian cancer.
The Importance of Screening Early Detection and Improved Prognosis
Ovarian cancer often presents with nonspecific symptoms in its early stages, making it challenging to diagnose. By undergoing regular screening tests, women have a better chance of detecting ovarian cancer at an early, more treatable stage. Early detection significantly improves the prognosis and increases the chances of successful treatment.
High-Risk Groups
Certain individuals have a higher risk of developing ovarian cancer and may benefit from proactive screening. High-risk groups include women with a family history of ovarian or breast cancer, those with known gene mutations (BRCA1 and BRCA2), and individuals who have previously had breast, ovarian, or colorectal cancer.
Available Screening Methods Transvaginal Ultrasound
Transvaginal ultrasound is a commonly used screening method for ovarian cancer. It involves inserting a small ultrasound probe into the vagina to obtain images of the ovaries. This non-invasive procedure helps identify any abnormal growths or cysts that may require further investigation.
CA-125 Blood Test
The CA-125 blood test is utilized to determine the concentration of a protein known as CA-125 in the bloodstream. Elevated CA-125 levels can indicate the presence of ovarian cancer, although it is not specific to this disease. This test is often used in conjunction with other screening methods to improve accuracy.
Risk Assessment and Genetic Testing
For individuals with a family history of ovarian or breast cancer, genetic testing can provide valuable insights into their risk of developing ovarian cancer. Individuals can make informed decisions about screening and preventive measures by identifying specific gene mutations, such as BRCA1 and BRCA2.
Screening Guidelines Age and Frequency Recommendations
The age at which ovarian cancer screening should begin and the frequency of screening depend on various factors, including personal and family history. In general, most guidelines recommend starting regular screening around the age of 40 or 50 and continuing until the age of 75, unless other risk factors are present.
High-Risk Individuals
For women at high risk due to family history or genetic mutations, screening may be recommended at an earlier age and conducted more frequently. Healthcare providers will assess individual risk factors and tailor screening recommendations accordingly.
Benefits and Limitations of Screening
Screening tests have the potential to detect ovarian cancer at an early stage when treatment options are more effective. Early detection can lead to better outcomes and improved survival rates. Regular screening may also identify benign conditions or non-cancerous cysts, providing reassurance to individuals.
False-Positive Results and Anxiety
Ovarian cancer screening can sometimes produce false-positive results, indicating the presence of cancer when none is actually present. False-positive results can cause anxiety and may lead to unnecessary
invasive procedures or surgeries. It’s important for individuals to discuss the benefits and limitations of screening with their healthcare providers.
Factors to Consider
Personal and Family History
Individuals with a family history of ovarian or breast cancer are at higher risk and should consider discussing screening options with their healthcare providers. They may be referred to genetic counseling or offered genetic testing to determine their individual risk profile.
Genetic Predisposition
Known genetic mutations, such as BRCA1 and BRCA2, significantly increase the risk of developing ovarian cancer. Individuals with these mutations should consider proactive screening and explore risk-reducing options such as prophylactic surgeries.
Surgical Interventions
Some individuals may have undergone surgical procedures, such as tubal ligation or hysterectomy, which reduce the risk of ovarian cancer. However, it’s important to note that these procedures do not eliminate the risk entirely, and screening may still be recommended based on individual circumstances.
The Role of Healthcare Providers
Discussing Screening Options
Women should have open and honest discussions with their healthcare providers about their individual risk factors, concerns, and preferences regarding ovarian cancer screening. Healthcare providers can guide patients through the available options and help them make informed decisions.
Shared Decision-Making
Shared decision-making is a collaborative process between patients and healthcare providers to determine the best course of action based on individual circumstances. This approach ensures that patients are actively involved in their healthcare decisions and have a thorough understanding of the benefits and potential risks of screening.
Ovarian Cancer Prevention Strategies
Lifestyle Modifications
Maintaining a healthy lifestyle can help reduce the risk of ovarian cancer. Engaging in regular physical activity, maintaining a balanced diet rich in fruits and vegetables, and avoiding tobacco use can contribute to overall well-being and lower the risk of developing various cancers, including ovarian cancer.
Oral Contraceptives
Studies have shown that the use of oral contraceptives (birth control pills) can reduce the risk of ovarian cancer. Women should discuss the potential benefits and risks of oral contraceptives with their healthcare providers to determine the most suitable options for them.
Risk-Reducing Surgeries
For individuals at high risk of ovarian cancer, risk-reducing surgeries such as bilateral salpingo-oophorectomy (removal of the ovaries and fallopian tubes) may be considered. These surgeries significantly reduce the risk of developing ovarian cancer but should be carefully discussed with healthcare providers due to their potential impact on fertility and hormonal balance.
Conclusion
Ovarian cancer screening is a vital component of women’s healthcare, offering the opportunity for early detection and improved outcomes. By understanding the available screening methods, guidelines, and considerations, women can actively participate in their health decisions and take the necessary steps to protect themselves. Consult with your healthcare provider to assess your risk factors, discuss screening options, and determine the best approach for your individual circumstances.
FAQs (Frequently Asked Questions)
FAQ 1: Is ovarian cancer screening 100% accurate?
No, ovarian cancer screening is not 100% accurate. While screening tests can help detect potential abnormalities, they can also produce false-positive or false-negative results. It’s important to discuss the benefits and limitations of screening with your healthcare provider.
FAQ 2: Are there any symptoms of ovarian cancer I should watch out for?
Ovarian cancer often presents with vague symptoms that may resemble other less severe conditions. These symptoms may include abdominal bloating, pelvic pain, frequent urination, and changes in bowel habits. If you experience persistent or worsening symptoms, consult your healthcare provider for evaluation.
FAQ 3: Can ovarian cancer be prevented?
While ovarian cancer cannot be entirely prevented, certain risk-reducing strategies can lower the chances of developing the disease. Lifestyle modifications, oral contraceptives, and risk-reducing surgeries may be considered based on individual circumstances and risk factors.
Learn more about – Cancer Prevention – Is It Possible?
FAQ 4: Are there any alternative screening methods for ovarian cancer?
Transvaginal ultrasound and the CA-125 blood test are the most commonly used screening methods for ovarian cancer. Alternative methods, such as pelvic exams or tumor markers, have limited effectiveness as standalone screening tools.
FAQ 5: How often should I undergo ovarian cancer screening?
The frequency of ovarian cancer screening depends on individual factors, including age, family history, and genetic predisposition. It’s essential to discuss screening guidelines and recommendations with your healthcare provider to determine the most suitable screening interval for you.
Learn more about Ovarian Cancer