Uterine Sarcoma: Understanding a Rare but Important Cancer
Uterine sarcoma is a relatively rare form of cancer that affects the uterus. Though it accounts for only a small percentage of uterine cancers, its impact can be severe. Understanding this type of cancer, its symptoms, risk factors, and treatment options is essential for early detection and improved outcomes.
-
What is Uterine Sarcoma?
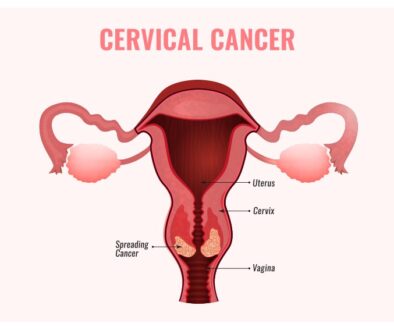
Uterine sarcoma is a type of malignant tumor that originates in the uterus’s smooth muscle or connective tissue. Unlike more common uterine cancers, which originate in the endometrium (lining of the uterus), uterine sarcoma arises from the supporting tissues of the uterus. The rarity of this cancer makes it challenging to diagnose and treat effectively.
-
Types of Uterine Sarcoma
There are several subtypes of uterine sarcoma, each with its own distinct characteristics. The primary types include:
a) Leiomyosarcoma
Among uterine sarcomas, leiomyosarcoma is the prevailing variety. It develops in the myometrium, the muscular layer of the uterus. This aggressive form of cancer tends to grow rapidly and may spread to other parts of the body.
b) Endometrial Stromal Sarcoma
Endometrial stromal sarcoma originates in the connective tissue cells of the endometrium. It is relatively less aggressive compared to leiomyosarcoma and has a better prognosis.
c) Adenosarcoma
Adenosarcoma is a rare type of uterine sarcoma that consists of both benign and malignant components. It usually affects younger women and may present with abnormal vaginal bleeding.
d) Undifferentiated Sarcoma
Undifferentiated sarcoma is a less common type and is characterized by its lack of specific differentiating features. Frequently, it is detected in its later stages, posing challenges for treatment.
-
Causes and Risk Factors
The exact cause of uterine sarcoma remains unknown, but certain risk factors may increase the likelihood of its development. These risk factors include:
- Age: Uterine sarcoma is more commonly diagnosed in women between 40 and 60 years old.
- Previous Radiation Therapy: Women who have received pelvic radiation therapy in the past may have a higher risk of developing uterine sarcoma.
- Hereditary Conditions: Some hereditary conditions, such as Li-Fraumeni syndrome, may predispose individuals to uterine sarcoma.
- Exposure to Tamoxifen: Long-term use of tamoxifen, a medication used to treat breast cancer, may be associated with an increased risk of uterine sarcoma.
-
Symptoms and Diagnosis
The symptoms of uterine sarcoma may mimic those of other uterine conditions, making it challenging to diagnose early. Common symptoms include:
- Abnormal vaginal bleeding or smelly discharge
- Vaginal bleeding is unrelated to post-menopausal bleeding or periods
- Pelvic pain or pressure
- Constipation
- Enlargement of the uterus
- The feeling of fullness in the abdomen
- Frequent urination
If uterine sarcoma is suspected, the following diagnostic tests may be performed:
- Transvaginal Ultrasound: This imaging test uses sound waves to create pictures of the uterus, helping identify any abnormalities.
- Endometrial Biopsy: A sample of tissue is taken from the lining of the uterus and examined for cancer cells.
- MRI or CT scan: These imaging techniques provide detailed images of the uterus and surrounding structures, aiding in the diagnosis and staging of uterine sarcoma.
-
Treatment Options
The treatment for uterine sarcoma depends on various factors, including the type and stage of the cancer, the patient’s overall health, and their preferences. The main treatment modalities include:
a) Surgery
Surgery is the primary treatment for localized uterine sarcoma. The surgeon may perform a hysterectomy, which involves removing the uterus and sometimes surrounding tissues and lymph nodes. For instance, total hysterectomy with salpingo-oophorectomy (the uterus is removed along with one or both ovaries or fallopian tubes)
b) Radiation Therapy
Radiation therapy employs high-energy rays to specifically target and eliminate cancer cells.
It may be used before surgery to shrink the tumor or after surgery to reduce the risk of recurrence. Radiation therapy can be both internal and external.
c) Chemotherapy
Chemotherapy involves using powerful medications to kill cancer cells or stop their growth. It may be used in advanced stages of uterine sarcoma or when the cancer has spread to other parts of the body.
d) Hormone Therapy
Hormone therapy is used for low-grade endometrial stromal sarcoma, as this type of cancer may respond to hormonal treatments.
Frequently Asked Questions (FAQs)
Q1: What are the survival rates for uterine sarcoma?
The survival rates for uterine sarcoma vary depending on the stage at which it is diagnosed and the type of sarcoma. Generally, early detection and treatment lead to better outcomes. However, the overall five-year survival rate for uterine sarcoma is around 50%.
Q2: Can uterine sarcoma be prevented?
There are no specific measures to prevent uterine sarcoma completely. However, regular gynecological check-ups and reporting any unusual symptoms to a healthcare professional can aid in early detection and better treatment outcomes.
Q3: How is uterine sarcoma different from endometrial cancer?
Uterine sarcoma and endometrial cancer are two distinct types of uterine cancers. Uterine sarcoma arises from the supporting tissues of the uterus, while endometrial cancer originates in the endometrium (lining of the uterus). The treatment approaches and prognosis for these two cancers differ significantly.
Bottom Line
Uterine sarcoma is a rare yet critical form of cancer that affects the uterus. Detecting cancer in its early stages and providing suitable treatment is vital for enhancing patient outcomes. If you or someone you know experiences any symptoms related to uterine sarcoma, consult an oncologist. Regular check-ups and awareness are essential to combat this disease effectively.